Report: ASHOT ZOHRABYAN
The Bio Prevention of Infections in War Related Injuries in the Republic of Armenia
INTRODUCTION
The necrosis and bacterial infestation of chronic wounds caused by nowadays firearms or explosive mines create a serious medical dilemma for the Army of the Armenian Republic. These wounds are characterized by extensive tissue damage, by massive destruction not only of the affected area, but also of the surrounding tissues, critical levels of bacterial colonization, and dysfunction of the microcirculation within the sphere of molecular shock. This is due to the molecular devastation transmitted to the wound’s surrounding tissue and thus the formation of secondary necrosis zones; these new zones of necrosis allow for intensive colonization by anaerobic microorganisms. The situation is further complicated by the formation of long lasting necrotization and suppuration. Despite the employment of present day, complex and combined surgical treatment and intervention procedures, approximately 15-20% of firearm wounds are still subject to severe complications caused by liquefy necrosis and early onset infections. Therefore, due to the problems associated with current medical protocols for firearm wounds, an alternative method of treatment should be considered.
PURPOSE
The application of larval therapy(LT,MDT) has advanced rapidly in recent years as its utility in treating wounds, including burn injuries. In developing countries, any strategy for rearing maggots will probably require equipment, maintenance, and minimum labor costs.
Adequate wound debridement, by surgical or non-surgical means, is a prerequisite to healing.
Nonsurgical debridement is generally slower; however, when surgery is not available or not a clinical option, LT can be an effective alternative. It is relatively rapid and very precise; larval scavenging of bacteria reduces infection, including that due to bacterial species resistant to antibiotics; local separation of gangrenous tissue, for instance in a diabetic foot, can postpone or even forestall major ablative surgery to the limb; LT can be undertaken in the community as well as in hospital.
CURRENT MEANS OF TREATMENT AND SURGERY
The basic prophylaxis of the further contamination of such wounds, until now, has been surgical treatment. Typically, wounds are subjected to:
·physical and chemical processing (ultrasound cavitation, enzyme preparations and others)
·the local treatment of the wound with the use of modern bandaging methods after primary surgical processing of the wounds
·targeted antibiotic therapy
·repeated surgical interventions
Early prophylaxis of purulent, liquefy wounds is imperative. The treatment of developed wounds is often complicated, laborious and costly, and often the results aren’t always satisfactory. Therefore it is fundamentally important that in such cases methods of prevention are rapidly implemented.
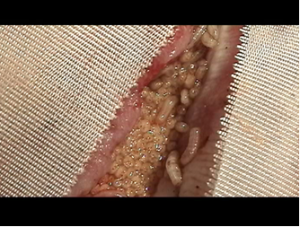 the latest bandage with the biomaterial before removing
the latest bandage with the biomaterial before removing
The main method of prophylaxis for firearm wounds, early infections has traditionally been the maximal excision method. This method includes a complicated set of procedures, which involve the removal of detritic and necrotic tissues, continual drainage of the wounds, regular administration of large quantities of assorted antibiotics and maintenance of conditions, which would prevent auxiliary bacterial infestation of the open area, all while encouraging the healing potential of remaining healthy tissue. Although this is the most prevalent method used for the treatment of firearm wounds, there are several drawbacks associated with it. These shortcomings include the high probability of improper tissue excision, which leads to the removal of viable tissue mass; this not only fosters the exacerbation of necrotic tissue development, but also causes additional physical trauma to the patient and requires the costly and time-consuming assistance of qualified medical personal specializing in battlefield surgery. Throughout the duration of it’s implementation, the primary excision method has led to several cases of secondary bleeding, manifestation of associated secondary disorders, enlargement of non-healing wounds, functional disorders and physical and psychological trauma to the patient.
In practice, there are several dynamics, which can lead to the inadequate implementation of a complete primary surgical treatment. They may include:
- Haphazard levels of damage caused to the tissues in the case of firearm caused wounds and the illegible border between viable and unviable tissues
- Absence of an objective method of early diagnosis or otherwise of an accurate evaluation of the viability of the damaged tissues
- Complex morphology of the firearm caused wound
- Specificity of the given anatomical sphere
Therefore, a more promising method of chronic wound treatment has been put into practice, the biosurgical method (maggot therapy). Live larvae of the species Lucilia Sericata (the common green bottle fly) are introduced to the wounds, they soon initiate a process of extracorporeal digestion, removing all of the necrotic tissue within a few days with extraordinary precision. The maggots purge the wound of unviable tissues and greatly reduce microbial contamination. They are natural necrophages, which feed exclusively on the wound’s detritic material include antibiotic resistant bacteria, without harming any healthy tissue. By means of a complex oral apparatus and by secreting a range of proteolytic enzymes, they liquefy the necrotic tissue and absorb the remaining liquid within a few days. . This enzymatic secretion gives an immediate bactericidal effect , one which has been proven effective even against several strains of resistant bacteria. For the biosurgical method, larvae are cultivated under laboratory conditions, and their growth has been accelerated by the use of a new and improved growing medium.
Justification for the prophylaxis of wound infections
 complete epithelialization after 1.5 months
complete epithelialization after 1.5 months
The biological significance of the processes taking place within each wound consists of a rational means of recovery, provided by nature. The increase of proteolytic activity accelerates the enzymatic cleavage of unviable tissues. A certain number of microbes-saprophytes also operate in the same manner, though by using of their own proteolytic systems.
Based on the knowledge that the medical community has to date about the essence of wound inflammation and the physiological processes of wound recovery, we can choose a proper treatment for firearm wounds. Instead of focusing on wound inflammation, it has been proven clinically more effective to: promote physiological healing procceses, remove necrotic tissues and the prevent colonization by pathogenic flora. Clinical studies for firearm wounds reveal that it is absolutely necessary to accelerate the proteolysis of necrotic tissues, while refraining from damaging healthy surrounding tissues. It is essential that these steps are taken in order to achieve the successful healing of the affected area.
The methodology of the bio-prevention(prophylaxis) of a wound infection:
- The preliminary minimized performance of a surgical intervention of the wound – excision of the extensively and visibly crushed tissues and opening of profound pouches necessary for aeration of the tissue
- Execution of rigorous homeostasis
- Immersion a biological preparation into the firearm wound
- Imposition of a breathable bandage
- Change the bandage every 3 to 7 days depending on the medical situation of the wound
Results demonstrated after the use of the bio-surgical treatment method:
- Improvement of treatment results, as well as the reduction of the period necessary for the recovery of the wounds
- Decreased needs for assistance of qualified medical personnel
- The elimination of need for the often monitoring and massive use of antibiotics
- Decrease of the expenses bandaging materials and other medications
- There is no further need for additional intervention, since the maggots (larvae) placed within the wound are actively and permanently at work
- The wound doesn’t needs new bandaging no earlier than 3 days
- No complications have been observed during treatment
Case report
Focal osteomyelitis of the calcaneus after a mine explosion injury. Admitted to hospital after 18 months of unsuccessful treatment and ported four operations. Constant fetid pus. Was imposed 4 biomaterial dressings for 10 days to complete wound cleansing. Epithelialization (cuticularization)of the wound has been completed after 1.5 months. Images: a - before using of biomaterial, b - the latest bandage with the biomaterial before removing , c and d - complete epithelialization after 1.5 months.
Conclusion
The implementation of bio-surgical methodology (bio-prevention), for the prophylaxis of firearm caused wound infections is both a labor and cost effective substitute for traditional methods of surgical protocols. This method decreases expenses, diminishes the need for qualified medical personnel, decreases the wound’s healing period, while also producing more satisfactory recovery results. The bio-surgical method does not have any dangerous side effects.
Editor LTC Manvel Vardanyan
Chief of desk of organization of medical
services in outpatient and inpatient clinics
Military Medical Department of AF of RA
Date: 11/19/2018
Source: Medical Corps International Forum (3/2013)