Article: Rakesh Jetly OMM CD MD FRCPC Colonel Psychiatrist
Mental Health Services in the Canadian Forces
The health needs, including the mental health needs, of Canadian Forces (CF) military personnel are a priority for the Government of Canada and the CF. As such, significant investment has been made by the CF to ensure personnel receive the highest standard of mental health care possible wherever they serve. The Canadian Forces Health Services (CFHS) has spent the past decade revitalizing its mental health care programs as well as playing a key role in the cultural change that has occurred in the CF towards mental health and those that suffer from mental illness.
Current organizational structure of CFHS
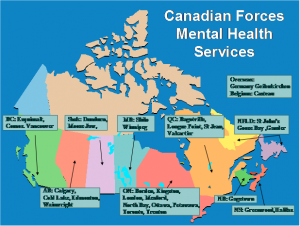 Canadian Mental Health Services
Canadian Mental Health Services
The CFHS is comprised of the Medical and Dental branches and provides a comprehensive continuum of health care and services to CF members at home, abroad and on deployed operations.
The organization consists of the Canadian Forces Health Services Headquarters and of intermediate headquarters strategically located across Canada to support the Health Services’ clinics and other units within their respective area of responsibility.
At the operational level, the Surgeon General provides guidance and direction on all aspects of health care in the CF including developing health care policy, setting standards, establishing procedures, and responding to issues from the field as they arise. He is the final authority on all health care issues and resolves disputes on professional issues between various groups of health care workers in the CF.
The Directorate of Mental Health reports to the Surgeon General and provides a single focus for all mental health-related activities and programs within the CF and DND. A senior Mental Health clinician is appointed as advisor to the D MH and chairs the Professional /Technical Advisory Group consisting of practice leaders for: psychiatry, psychology, social work, MH nursing, addictions and Health Service chaplains.
CF Mental Health Service Delivery
Today, there is a full range of mental health care services available to our CF members throughout all aspects of their career, from recruitment to retirement and throughout the entire deployment cycle, including pre-deployment, during deployment, and post-deployment. A CF member can at any time access his or her primary care clinician to address health concerns including those of a psychological nature. The mental health of CF members is continually being assessed through regular periodic medical check-ups that occur in primary care settings. Screening questions pertaining to post traumatic stress disorder (PTSD), depression, addiction, suicide, and other mental health conditions are routinely asked and issues are addressed. If further assessment or specialized treatment is required these can be provided by mental health professionals.
Mental Health care is delivered at CF Health Care Clinics (HCC) across Canada and abroad through an internal service delivery model and a cadre of external community providers. Currently, mental health programs are delivered by approximately 378 military and civilian mental health providers plus additional support staff. This is the highest ratio of providers to service members amongst our NATO allies.
CF Mental Health Services consists of two distinct services: Psychosocial Services and Mental Health Services. Psychosocial Services comprise a basic level of mental health care that is closely integrated with the primary care delivery unit (CDU) and is staffed by nurses, social workers and addictions counselors. This program provides for easy-accessible first-line care, for which no referral from a physician/Medical Officer (MO) is needed. This program is available at all CF clinics. The secondary level of service, Mental Health Services, consists of specialized programs such as: the Operation Trauma and Stress Support Centre (OTSSC) program which focuses on the treatment of operational injuries, the MH program which focuses on general MH conditions and the Addiction program. For these programs a referral of a physician/MO is required. Service is provided by an interdisciplinary staff of psychologists, psychiatrists, Mental Health nurses, social workers, addictions counselors and Health Services chaplains. These secondary programs are located at the larger centres and have a regional responsibility. The whole MH system includes national level co-ordination and strategic assessment and planning capability and is capable of deploying interdisciplinary MH teams as needed in support of deployed operational elements of the CF.
Additional CFHS programs available to CF members
The Canadian Forces Member Assistance Program (CFMAP) was established in 1999. It is a voluntary, confidential, short-term counseling service, to help CF service members and their families who have personal concerns that affect their personal well-being and/or work performance. The Program is available 365 days a year, 24 hours a day, 7 days a week.
Strengthening the Forces (STF), the CF's health promotion program is designed to enable CF members to increase control over and to improve their overall health and well-being. The CF's Strengthening the Forces health promotion program includes four Core Program Areas: Addictions Awareness and Prevention, Injury Prevention and Active Living, Nutritional Wellness, and Social Wellness. Social Wellness includes Suicide Prevention, Anger Management, Stress Management, Healthy Relationships, and Family Violence.
Deployment Health which is part of the Directorate of Mental Health was stood up to understand and to mitigate the adverse health consequences of military deployment in Canadian Forces (CF) members, with a particular focus on mental health problems and Medically Unexplained Physical Symptoms [MUPS] and other injuries such as Mild Traumatic Brain Injury (mTBI) in Military Operational Settings. This is accomplished through a combination of research, education, and policy development.
CF Affiliated Programs
In addition to the delivery of direct MH care the CFHS works with other organizations within the CF focusing on Mental Health including:
The MH & Operational Stress Injury Education Advisory Committee (MH & OSI EAC) that was appointed to provide CF members (all levels) and their families with education, training and awareness sessions throughout the career-cycle to promote their MH and well-being and to shift behaviors and attitudes towards MH. The MH & OSI EAC is the CF coordinating body for review, assessment and approval of all (non-clinical) MH training and education initiatives targeting CF members and their families, prior to its implementation.
The Operational Stress Injury Joint Speakers Bureau (OSI JSB) affiliated to MH & OSI EAC was also established in 2007. It develops, delivers and evaluates MH education across all levels of the CF, including CF members’ families. The education of the OSI JBS is focused on pre- (and post-) deployment intervention. Features of the OSI JBS program are that it uses two types of speakers, i.e. peers and professionals; there is a great focus on teaching the CF leaders; also, a good family system is emphasized, therefore family members are also included in the program.
The Operational Stress Injury Social Support (OSISS) is a peer support network of former operational stress injuries survivors. It has taken on a key role in trying to eliminate the stigma of MH illness through education and outreach to the general CF population as well as the Chain of Command. The peer support coordinators (PSC’s) of the OSISS, who receive mandatory training, work closely together with the MH professionals of the OTSSCs and with OSI JSB (mentioned above).
The Military Family Resource Centres (MFRCs) are located on all CF bases across Canada and where CF members are located abroad. These centres are dedicated to enhancing the quality of military family lives by the provision of unique services tailored to the military community, including: helping families of CF members manage the stresses associated with the military lifestyle. Programming includes education and support related to deployments, individual and family counselling, child care, language education and assistance in seeking employment.
Expert panels are also conducted on an as need basis. In 2008 an expert panel met on the Management of Mild Traumatic Brain Injury (mTBI) in Military Operational Settings. The goal of the panel was to undertake a careful review and critical appraisal of the available evidence on mTBI in a military operational setting in order to recommend a strategy for the surveillance and management of this in Canadian Forces personnel in military operational settings that is balanced, feasible and logical given the available evidence. The panel consisted of persons with expertise in emergency medicine, trauma medicine, psychiatry, internal medicine, neuropsychology, rehabilitation medicine, epidemiology and basic science. Most of the panel consisted of Canadian Forces medical personnel with operational experience. Outside experts in the fields of neuropsychology as well as international guest speakers from the United States Army and the United Kingdom Ministry of Defence also participated.
In 2009 an international expert panel on Suicide Prevention was convened to examine population based suicide prevention programs and clinical practices that may make a difference in everyday practice in the Canadian Forces. The panel confirmed that the CF has a strong and comprehensive suicide prevention program that compares favourably with those of its closest allies, including the US Air Force’s benchmark program. Nevertheless, the Panel did identify some opportunities for reinforcing the CF’s program, most notably the need to improve its ability to systematically improve the quality of mental health care that it delivers. Given the strength of the CF’s existing program, the panel’s recommendations represent additional prevention opportunities to exploit as opposed to serious deficiencies to correct.
 MH Support Activities Pre and post deployment
MH Support Activities Pre and post deployment
The CF recognizes the need for a robust pre and post deployment mental health program in order to ensure CF members and their families are equipped for the stressors associated with deployment. MH support prior to deployment focuses on three main areas, the first is the mission specific assessment of the MH support requirement, secondly pre-deployment screening and thirdly pre-deployment education and training of CF members and families.
Mission specific assessment
Mental Health requirements for deployments are assessed for all missions. The number of military MH personnel deployed, will be determined by the nature of the mission, the number of troops being deployed, the length of the mission, expectations of MH services required and the availability of services from our allies/local resources. The CF continues to monitor all factors related to the mission and deploy the appropriate interdisciplinary resources. For the mission in Afghanistan, mental health providers included a psychiatrist, MH nurse and Social Worker for each rotation.
Pre-deployment screening
Prior to deployment every member undergoes a mission specific pre- deployment medical and psychosocial screening. The medical screening which is conducted by a medical officer is done to ascertain the member’s medical fitness to ensure that personnel deploying on a mission are fit to carry out their tasks. A psychosocial screening involves an interview with a social worker and may include the member’s spouse to examine the impact the deployment may have on the member and their family as well as whether or not there are personal or family circumstances precluding the member from deploying. Based on this information recommendations are made to the member’s Commanding Officer as to the member’s suitability for deployment.
Pre-deployment training
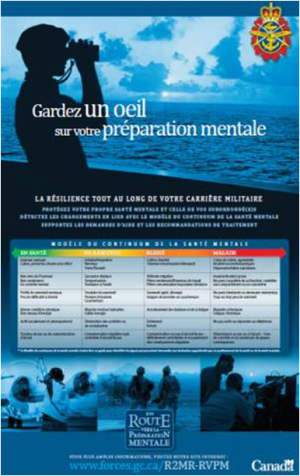
Mental Health education is delivered continuously throughout a member’s career. For each deployment training is delivered which focuses on: understanding stress reactions; identifying challenges of deployment and their impact; learning and applying strategies to mitigate the impact of stress; and, recognizing when and where to seek support. This training which is known as the Road to Mental Readiness aims to prepare servicemen, leaders and their families to identify and meet the challenges related to deployed operations and geographical family separation. The program has its roots in sports performance psychology, and applies goal setting, visualization, self-talk and arousal control to mitigate the body’s automatic physiological reactions in situations of extreme stress and fear. The skills, referred to as ‘The Big 4’ are taught briefly in a classroom environment, and then coached in a simulation/exercise where there is some element of stress. The long term intent is to incorporate these skills into MH education at different carrier levels and simply apply them to pre-deployment situations. The training is delivered by a trained deploying CF member and an experienced CF MH professional. The commander also takes an active role in reinforcing the importance of this training.
MH support in theatre
Support in theatre is provided by an interdisciplinary team, minimally a MH nurse, a social worker and a psychiatrist are available to offer support to deployed soldiers. These three professions form the core of the MH care team and work in conjunction with Medical Officers and technicians. Additionally, chaplains are also available to provide assistance. The deployed MH team will focus on health promotion and prevention (through briefings) and will undertake assessment and treatment as needed. The vast majority of the work is individual and often involves Cognitive Behavioral Therapy (CBT) in conjunction with medication.
Post-deployment MH support
The CF has introduced a decompression period as part of the total reintegration process for CF members returning from Deployment. The reintegration process consists of several phases: preparation (in theatre, 2-4 weeks before leaving), decompression (at a third location), a reception (at home) and post deployment follow-up (3 - 6 months after return). After third location decompression (TLD) the unit returns to their home base and members go back to work for 3 half days before being allowed to go on a leave. This is implemented as an additional “decompression” in order to make an optimal transition to home/base life.
Decompression
There are two major components to the decompression program, one of which is educational and provided by mental health professionals from the Canadian Forces Health Services Group. The other is provided by Canadian Forces Personnel Support Agency and includes organized and self-directed recreation programs. These services, in combination with provision of a comfortable clean bed in a decent hotel room, privacy, and time to sleep and wind down, help with reintegration into both home and work life back in Canada. The mental health team is on site to provide educational information in support of reintegration into home, work and community life back in Canada as it is important for members to be aware of situations that may arise once they are home, back with family and into their normal workplace. Additionally, members are provided with general knowledge about operational stress injuries.
For each rotation the commander in theatre decides if their group requires TLD. There is a set of criteria which is considered, including: the level of deployment hardship, risk and operational tempo; occurrence of traumatic incidents; duration of the deployment; type of Rest and Recreation (R&R) or mission leave; and communication with the family. For the mission in Afghanistan the practice was for all Canadian troops to undergo TLD.
Post –deployment screening
The “Enhanced Post-deployment Screening Process” has been required of all members returning from an operational deployment of 60 days or more since 2003. The enhanced process helps to identify individuals who otherwise may not have come forward or who may not have even recognized potential mental health issues in themselves. It allows for early intervention and where significant progress is most likely to result. Many members with a broad range of previously unrecognized mental and physical health problems have been identified through this screening process, and our members have evaluated it very favourably. The process takes place 3 - 6 months after their return and consists of: the member completing a detailed, validated health questionnaire covering relevant deployment-related mental and physical health problems, PTSD among them; and undergoing a 20 – 40 minute semi-structured interview with a mental health professional (usually a social worker or mental health nurse). The interview touches on any abnormal responses on the questionnaire, and it also includes a number of open-ended questions on family and social reintegration.
Date: 11/01/2018
Source: Medical Corps International Forum 2/2013