Article
Communication Improves Diagnosis and Therapeutic Management in a Simulation-Based Scenario
The aim of this study was to examine whether communication skills have an influence on diagnosis and therapeutic management in a simulation-based scenario. Forty anesthesiologists were exposed to a clinical malignant hyperthermia (MH) event. Their performance was videotaped for a retrospective analysis. Communication was categorized to determine the quantity and quality. The quantity of the communication, demographic variables or clinical experience did not influence diagnosis and therapeutic management. The participants showed communication skills of higher quality by presenting more closed loops, diagnosed and managed the MH crisis more quickly.
Introduction
Anesthesia crisis resource management (ACRM) is a well-established method for dealing with critical situations.1–4 There are several key principles in ACRM behaviors – also known as non-technical skills (NTS) – such as anticipation and planning, communication, leadership and assertiveness, the use of all available resources, re-evaluation of situations and the use of all available information and cross checking of redundant data.5
One key aspect of ACRM is (verbal) communication, an important tool for exchanging information particularly in critical situations.1,3 A substantial number of indices demonstrate that communication skills might have a positive effect on medical practice.1–4 For example, in an emergency room for a few weeks all conversations were recorded. It was found that in many cases, the communication during trauma resuscitation was suboptimal.6 Furthermore, Arbous et al. showed that inadequate communication is a major risk factor for mortality associated with anesthesia and was attributable for 25% of all anesthesia related deaths in an analysis of 869483 anesthesia.7 Communication most likely has a significant relevance to incidents and their management in medicine.8,9
Physicians, such as anesthesiologists, do not ignore the importance of communication skills in their practice.8,9 Weller et al. systematically reviewed the changes in practice following a simulation-based training in crisis management.10 They showed that the key learning points obtained from simulation-based training were communication skills. These skills were outstanding reasons for increased confidence following simulation-based training in the ability to manage a crisis. Despite the hypothesis that communication in critical situations is important, there is little data available because the effects of communication are difficult to measure. 4,11,12
The following study analyzes the effect of communication on crisis management in a simulation-based scenario. We hypothesized that high qualitative and adequate communication skills would lead to accelerated diagnosis and therapy.
Methods
Design of Study
Forty anesthesiologists from two academic hospitals and five local hospitals served as participants in the test. The inclusion criteria were anesthesiologist, anesthetic experience >6 months, no past participation in simulation-based NTS training at any center before, willingness to participate during the participants’ spare time on a voluntary basis, and not exceptionally experienced in crisis management. Parts of the data used in this study are based on a former inquiry.4 The study was approved and conducted at the Medical Faculty of the University of Heidelberg. Approval by an ethics committee was not necessary.
Scenario
The scenario was based on a young patient with typical symptoms of acute appendicitis, who was transferred to the operating room for an appendectomy. The participants conducted anesthesia and decided on the pharmaceuticals to be administered and the medical tasks. The members of the simulation team played the roles of surgeon and surgical and anesthetic nurses.
Intraoperatively, the patient presented typical symptoms of MH that could be described as inadequate relaxation, a progressive increase of FeCO2, tachycardia, arrhythmia, desaturation, (if ordered) a BGA showing respiratory and metabolic acidosis with hyperkalemia, increasing body temperature, and progressive hemodynamic and pulmonary deterioration. The scenario was based on a typical clinical presentation of MH.13 The sequence, the occurrence and the intensity of symptoms were identical for every participant throughout the study. The symptoms that could not be simulated for technical reasons were presented (e.g., by the surgeon „the skin is warm, does the patient has temperature?”) to the participants at a predefined time in the scenario.13,14
Data Analysis
Demographic data of the participants was obtained including the age, sex, clinical experience, simulation experience, board certification, and current employer. The scenario was audio/videotaped for a retrospective analysis. The time was registered via an integrated stopwatch. An evaluation sheet was developed and used to note the vital parameters, intraoperatively presented symptoms and administration of drugs (time and type of drug). As decisive steps towards a successful treatment of the MH, special focus was set on the elimination of the trigger, the order of a blood-gas-analysis (BGA) and therapy with a dantrolene infusion.
The communication skills were recorded and classified as follows: The exact wording of each sentence of each person in the scenario was noted. The communications were distinguished between the senders and receivers including the participants, nurses, surgeon and persons on the other end of the telephone communication. The communication categories were as follows: second opinion, question, information and instruction (table 1).15,16 The frequency of each category determined the quantity of the communication. To determine the quality of the communication, the following four characteristics were checked for each category: the quality of a request, answer and reaction as well as performance of a „closed loop” (table 2).17,18 One point was given for each specific information item, inquiry or answer; for every „closed loop”; and for medical relevance. Only the communication skills of the participants (anesthesiologists) were analyzed.
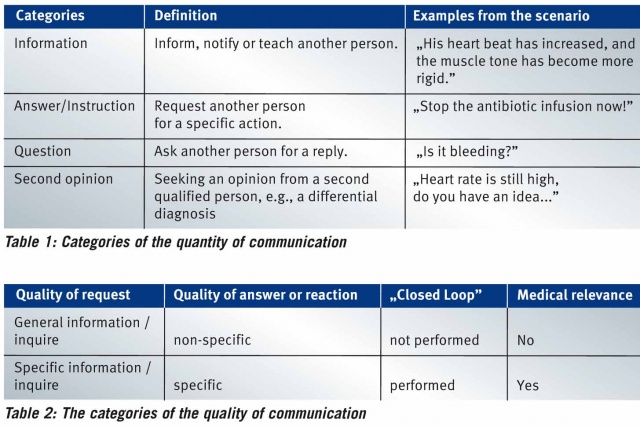
For more effective visualization, we further categorized communication skills as „high”, „intermediate” and „low” quality communication skills by the following definitions: „high”, participants presenting quality communication in >50% of the total communication; „low”, participants presenting quality communication in < 30% of the total communication; and „intermediate”, participants presenting quality communication in 31–49% of the total communication.
The videotapes were separately analyzed by two experienced members of our team, who were not involved in the planning or realization of the experiment.
Statistics
The interrater reliability was calculated from ten videos using the intraclass correlation coefficient (ICC). A value of 0.0 indicates agreement between the raters at the level of chance, and 1.0 indicates perfect agreement. The level of agreement was calculated as a proportion of the overall agreement and the proportion of agreement specific to each phase of the scenario.
The vital parameters, appearance of MH symptoms, and each diagnostic and therapeutic step by the participants were registered and chronologically recorded. Each scenario was normalized with regard to the beginning of the operation procedure („skin incision”, see below). The quantity and quality of communication were noted on the evaluation sheet. After completion of the data acquisition, the data were collected into an electronic database and analyzed using Microsoft Excel (Microsoft Office Professional Plus 2010, Microsoft, Redmond, USA) software. The analysis of the groups regarding the significant differences was performed with the t-test for normally distributed data. The calculation for the non-normally distributed data was performed using the U-test (Whitney-Mann). For the statistical calculation, SPSS software was used (SPSS Version 11, IBM, Armonk, USA). P < 0.05 was considered statistically significant. If not stated elsewhere, the presented data in the tables and figures are the mean and standard deviation.
Results
Characteristics of the Participants
A total of 36 videos of the 40 participants were analyzed in this study because four videos could not be evaluated, two because of technical problems and two because of a language factor (non- native participants). There were 20 males and 16 females, and the average age was 32 (range: 27 – 50) years, the duration of clinical experience was 3 (range: 0.5 – 20) years, and 8 participants were board certified anesthesiologists.
Interrater Reliability
The ICC one-way random, average measure indicates strong agreement at 0.78 (P<0.001). We conducted an independent analysis of an observation sheet by two members of our team for 10 different videos.
The quantity and quality of communication
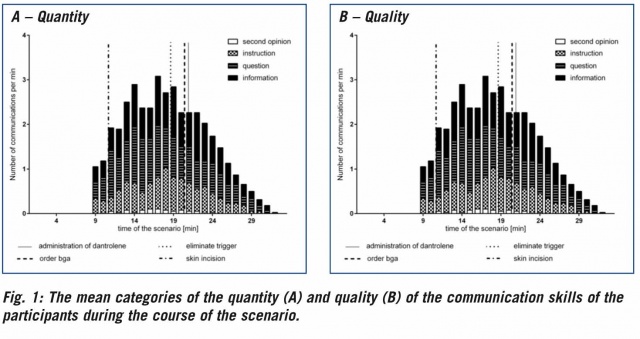
The mean of the quantity and quality of communication during the scenario are displayed in figure 1. On average, each anesthetist communicated 40 ± 11.5 times through the evaluated section of the scenario. The mean of the communication could be divided into 40% questions, 32% information, 25% instructions and 3% seeking a second opinion. During the course of the scenario, a change in the communication behavior could be observed. With the increase of the symptoms of MH, there was an increase in the number of communications of each category by the subjects (Figure 1A). On average, the number of communication events approximately doubled. This dynamic was observed for each participant. The mean of the quality of communication shows the identical trend (Figure 1B).
All of the participants diagnosed the MH correctly and eliminated the trigger. During the scenario, the skin incision was performed at 11.05 ± 2.08 min, the elimination of the trigger occurred at 19.20 ± 4.16 min, and the order of a BGA came at 20.95 ± 6.11 min. In total, 75% of the participants ordered a BGA. The administration of the dantrolene infusion occurred at 21.38 ± 4.59 min.
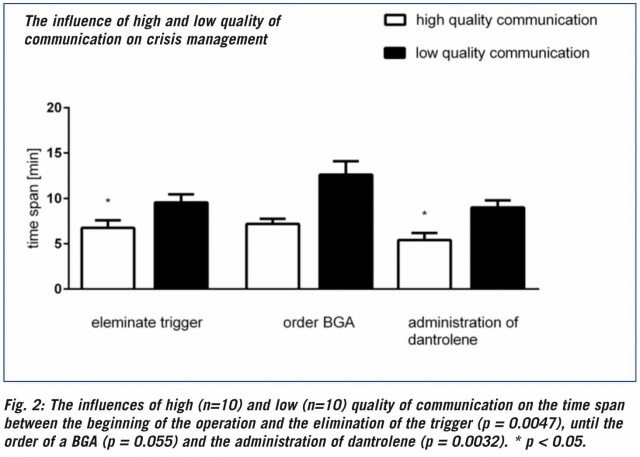
The comparison of the high (n=10), intermediate (n=16) and low (n=10) quality communication skills of the participants showed significant differences between the high and low quality groups (Figure 2). The participants with high quality communication skills showed an average of 7.2 ± 0.55 minutes from the skin incision to the order for dantrolene. The low quality-communicating participants ordered the drug significantly later (12.6 ± 1.49 min). The low quality-communicating participants showed a delayed removal of the trigger and order for a BGA.
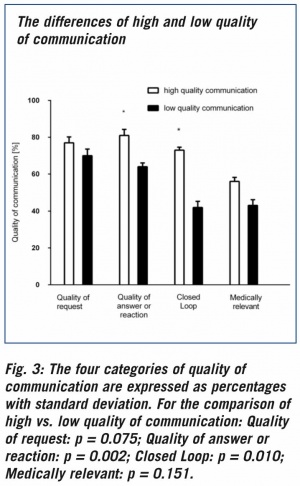
High quality communication was associated with a trend towards a higher frequency of qualitative requests and medical relevance, and it showed a significantly higher frequency of qualitative answers or reactions and closed loops (Figure 3).
Comparison of high and low quality groups: Gender (p = 0.603), clinical experience (p = 0.602), board certification (p = 0,877) and age had no influence (p = 0.247) on the time between the beginning of the operation and the administration of dantrolene. The demographic variables and the quantity of communication were not different between the high- and low-quality communication groups.
Discussion
The aim of this study was to investigate the effect of communication skills on crisis management in a simulated case of MH. We were able to demonstrate that communication plays a central role in crisis management, as the quantity and quality of communication increased with worsening of the crisis. In particular, high quality communication leads to a quicker diagnosis of and therapy in an MH crisis. Particularly, „closed loops” appear to play an important role in this scenario.
In the past, education based on medical core knowledge and basic skills was assumed to be essential and sufficient for medical training.19 However, evidence has grown, that other important domains are necessary for becoming a competent clinician who „possesses the integrative ability to think, feel, and act like a physician”.19 One dimension of this professional competence is basic communication skills. The fundamental function of communication is to transport information from a sender to a receiver. However, failure of communication is the basis for errors and complications, and it might endanger patient safety.3,11
Communication is particularly important in critical incidents, in which tasks are required to be arranged under time pressure and stress in an order of priority to reduce the patient’s risk.6,8 Cyna et al. describe that communication between medical personnel in an emergency represents a distinct challenge.20 Team members have different skills and characteristics, and the clinical problem might change during the course of the treatment. It is necessary that a physician selects the right type of communication under these circumstances.20 Communication requires a dynamic exchange of signals between the transmitter and receiver. Problems frequently arise because of a lack of or faulty communication skills.8,11
Communication quality appears to be important, and it is a key element, particularly, in critical incidents.8,15,21 We focused in this study on the quality of communication. One criterion of quality was the specificity or lack of specificity of a request, answer or reaction. Other studies have shown, the more commands are specific and directed, the more they are likely to be acknowledged and performed.22 An aimless instruction could result in a situation in which nobody feels addressed and no action is performed.23
Another criterion was the use of a closed loop. The closed loop concept, borrowed from aviation and applied to medicine, has a major effect on the handling of critical incidents.8 The concept consists of (verbal) feedback to ensure that the team colleague correctly understood or performed the message or instruction. In our study, the participants showing high quality communication skills showed more closed loops and specific answers and reactions. These results are comparable to other studies showing that high performing teams uses feedback more frequently than low performing teams.24 In trauma teams, the frequency of use of closed loops was significantly linked with professional experience.17 This correlation was not observed in our study. Clinical experience, age, gender, or the care level of the hospital could be hypothesized to have an effect on the speed of diagnosis or therapy of MH. However, no demographic variable showed an influence.
In this study, the clinical picture of malignant hyperthermia was simulated. This disease has been successfully used in a variety of other simulation-based incident studies and is an accepted scenario for the presentation and collection of technical and non-technical skills.4,14,25 We selected this scenario because anesthesiologists are familiar with the typical clinical symptoms and basic treatment of MH. Gardi et al. showed that untrained anesthesiologists and nurse anesthetists made the diagnosis of MH and determined the first basic steps of treatment correctly in 100% of the cases.14 These results are comparable to ours. To our knowledge, this study represents the first time that the quantity and quality of communication over the entire time course in a MH simulated scenario is presented.13,14 Because medical knowledge was not a handicap for our participants, the differences in the groups might be more explainable by NTS, specifically in this case by communication. It is unclear to what extent these results could be easily transferred into other (simulation-based) scenarios and whether an unrestricted transfer into medical practice might be possible. In addition, the question arises to what extent the MH incidence remains clinically significant because, through the introduction of total intravenous anesthesia and the decreasing use of succinylcholine, potential triggers for MH become rare, and thus the probability of the occurrence MH is decreasing.26
When considering the results, however, it should be noted that the data were collected retrospectively. Thus the number of videotapes was limited to 40. In addition, for technical reasons and because of the presence of non-native speakers, we reduced the number of evaluated videotapes to 36. We removed the non-native speakers from the analysis because they show different communication behaviors. We could not rule out whether this factor could have influenced our study results. The definition of our categories was based on former studies.27,28 We might have interpreted or reassigned these categories differently, making the direct comparison to other studies more difficult. Our interrater reliability was high, showing strong agreement and the stability of our categories in this simulation-based study.
Communication is a decisive factor for the successful management of a crisis. To improve the management of emergencies, communication should be optimized.21 Therefore, communication training is essential. 8,12,29 As an addition to such training, supervised simulation training is a very effective tool.13,14 The participants of simulation-based training report an improvement in their daily work, and, in particular, they improved their communication skills.10 For physicians, it is therefore convincing to employ high quality communication skills to learn, improve and practice. Our simulation-based study shows a strong relationship between the quantity and quality of communication and the worsening of a MH crisis. The participants who used more qualitative communication skills, particularly more closed loops, succeeded more quickly in diagnosis and therapy in a simulation-based study.
References: ref@mci-forum.com
Date: 09/28/2016
Source: MCIF 4/16